Inflammatory bowel disease (IBD),including ulcerative colitis (UC) and Crohn's disease (CD), is characterized by chronic relapsing intestinal inflammation of unknown etiology. Studies suggest that genetic, environmental, and immunologic factors lead to disruption of the intestinal mucosal barrier, causing the translocation of intestinal bacteria to the submucosa, which in turn triggers immune cell activation and intestinal inflammation. The chronic relapsing inflammation further inhibits intestinal epithelial repair and exacerbates the intractableness of IBD. The intestinal epithelial barrier repair depends on intestinal stem cells (ISCs), a population of Lgr5-positive cells located at the base of crypts. Regulated by niche signaling, Lgr5-positive stem cells proliferate and differentiate into mature absorptive and secretory lineages, which play a crucial role in epithelial cell renewal and maintenance of mucosal barrier integrity. The classical Wnt signaling pathway is a determining factor in maintaining ISC stemness, and studies have shown that M2 macrophages are an important source of Wnt in adult tissues, although their precise molecular mechanisms are not fully understood. Recent studies on IBD patients and mouse models suggest that impairment of ISC stemness is the key factor leading to the recurrent inflammation. Therefore, treatment for IBD should not only suppress inflammation but also restore ISC stemness to promote repair of the intestinal epithelium and restore mucosal barrier function. Currently, treatments for IBD, whether aminosalicylates, glucocorticoids, immunosuppressants, or biologics, can effectively control immune inflammation but have very limited effects on mucosal repair. There is still a lack of drugs that can promote mucosal repair. Recently, the research team led by Professor Xiaoyan Shen from School of Pharmacy, Fudan University discovered sorting nexin 10 (SNX10) as a novel potential drug target for IBD treatment. Intervention in this target can increase cholesterol synthesis, thereby restoring ISC stemness, promoting intestinal epithelial repair in IBD mouse models. The related work titled "Inhibiting sorting nexin 10 promotes mucosal healing through SREBP2-mediated stemness restoration of intestinal stem cells" was published online on August 30, 2023, in the journalScience Advances (PMID: 37647408, DOI: 10.1126/sciadv.adh5016).
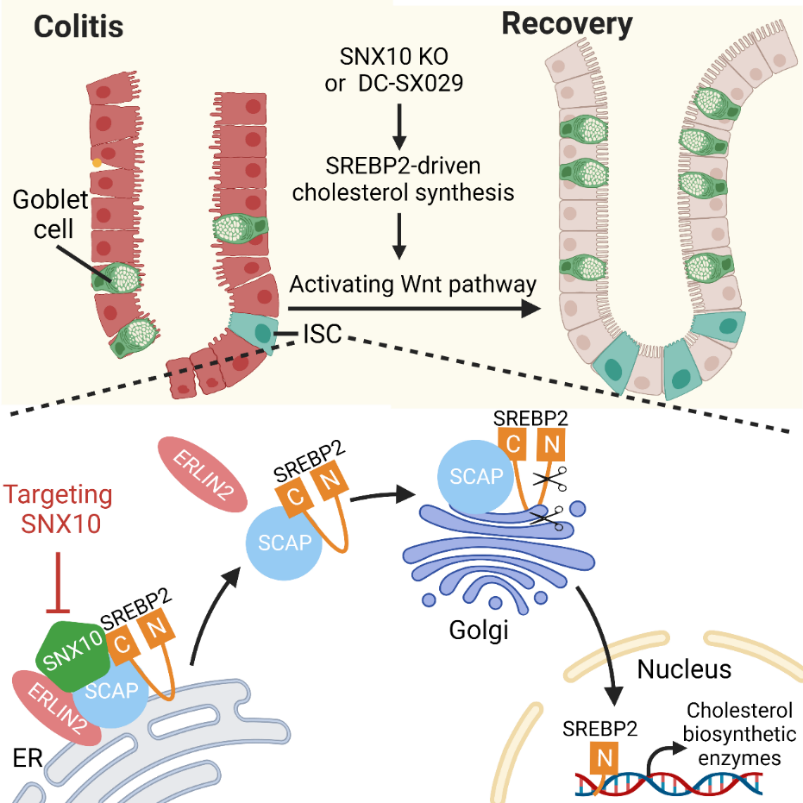
Mechanism Diagram: Anchoring of sterol regulatory element-binding protein 2 (SREBP2) to the endoplasmic reticulum (ER) by SNX10 prevents its transport and activation, resulting in decreased synthesis of intracellular cholesterol, which inhibits the proliferation and differentiation of ISCs in IBD. This process can be reversed by a small molecule inhibitor of SNX10 DC-SX029.
The research team found that the expression of SNX10 in ISCs is positively correlated with the severity of human CD and mouse colitis has determined by analyzing clinical data and animal studies. Specific knockout of the SNX10 gene in intestinal epithelial cells or ISCs promotes mucosal repair by restoring ISC stemness in mouse colitis models induced by dextran sulfate sodium salt (DSS) or 2,4,6-trinitrobenzenesulfonic acid solution (TNBS). Gene set enrichment analysis (GSEA) of sorted epithelial cells suggests that this stemness-restoring effect is associated with the activation of early cholesterol mevalonate pathway. In vitro organoid models confirm that SNX10 deficiency accelerates cholesterol biosynthesis, enhances cell sensitivity to WNT ligands, and thereby reinforces ISC stemness. Fluorescence live-cell imaging combined with immunoprecipitation experiments revealed that SNX10 deficiency dissociates the ER lipid raft associated 2 (ERLIN2) -SREBP cleavage-activating protein (SCAP) complex, and promotes the transport of SREBP2 from the endoplasmic reticulum to the Golgi apparatus for subsequent cleavage and activation.
The research team validated these mechanisms using a protein-protein interaction (PPI) inhibitor of SNX10, DC-SX029, which enhanced ISC stemness and promoted mucosal barrier restoration, demonstrating an excellent anti-IBD activity. These findings suggest that targeting SNX10 or other regulatory factors involved in SREBP2 activation or the axis of cholesterol metabolism may provide a new strategy for mucosal healing in IBD.
Postdoctoral fellow Weilian Bao, associate researcher Yan You and Ph.D. student Jiahui Ni are co-first authors of this article. Professor Xiaoyan Shen and Professor Daofeng Chen from School of Pharmacy, Fudan University, and Dr. Peng Du from Xinhua Hospital, Shanghai Jiaotong University School of Medicine, are the corresponding authors of the article. This research was funded by the National Natural Science Foundation of China and the Science and Technology Support Project of Shanghai Science and Technology Commission in the field of laboratory animals.
Original article link: https://www.science.org/doi/10.1126/sciadv.adh5016