脑卒中是全球致残率最高、致死率第二的疾病。由于脑供血动脉狭窄或闭塞造成的缺血性脑卒中占所有脑卒中病例的85%以上。血管再通是缺血性脑卒中首选治疗方案。重组组织型纤溶酶原激活剂(rt-PA)是目前FDA唯一批准用于临床的溶栓药物。但rt-PA具有严格的使用时间窗口(症状产生后4.5小时以内)。超过该时间窗口使用会导致脑出血、脑水肿等严重副作用。我国仅有5%的缺血性脑卒中患者能够受益于该药物。因此,对绝大部分失去溶栓治疗机会的患者实施有效治疗是目前亟待解决的临床问题。
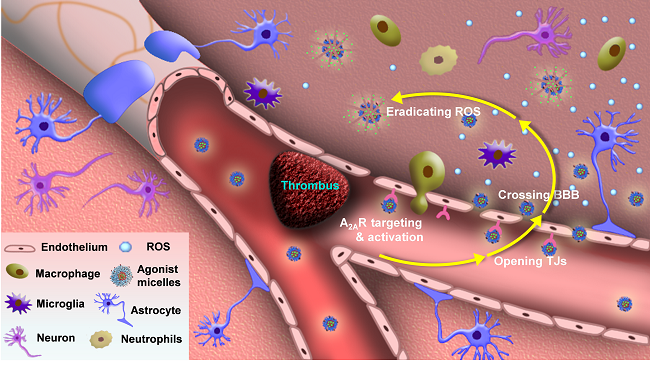
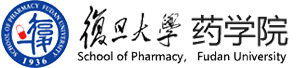
图1. 激动胶束主动调控血脑屏障通透性提高神经保护药物递送效率
神经保护治疗通过阻碍缺血后破坏性级联事件的发生,提高神经元存活率,改善神经功能。但绝大多数已报道的神经保护剂并未在临床实验中发挥显著疗效。血脑屏障阻碍药物入脑是上述神经保护剂疗效不佳的重要原因。在线发表于《Theranostics》杂志上的一项研究中(Edaravone-Encapsulated Agonistic Micelles Rescue Ischemic Brain Tissue by Tuning Blood-Brain Barrier Permeability),复旦大学药学院李聪教授研究团队报道了一种激动胶束,能够主动开启缺血区域血脑屏障并实现所包载神经保护药物的高效递送。
图2. 磁共振成像发现激动胶束提高缺血部位体积缩小
该研究第一作者、硕士研究生靳取介绍:该激动胶束内腔包载有临床使用的自由基清除剂依达拉奉,而表面修饰有腺苷2A受体激动基团。该激动胶束通过激活缺血区域血管高表达腺苷2A受体促进内皮细胞收缩、开启内皮细胞间的紧密连接,高效跨血脑屏障入脑。在缺血性脑卒中模型鼠中,与直接注射药物相比,该激动胶束显著提高依达拉奉在脑卒中区域的浓度,促进脑缺血区域体积减小并加快神经纤维束的恢复。李聪教授认为:该激动胶束同时实现了血脑屏障主动调控和药物递送,规避了大多数神经保护药物代谢速度快,循环周期短,使用剂量大等缺点。
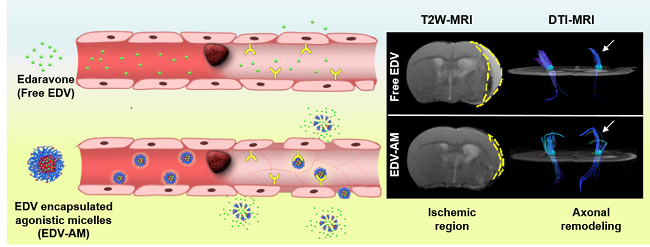
图3:激动胶束对加快缺血区域神经束恢复速度
本研究共同通讯作者,东南大学东大医院放射科居胜红教授认为:缺血/再灌注引发自由基过量产生贯穿于缺血性脑卒中的整个过程(急性期、亚急性期和恢复期),并与炎症、水肿、神经元凋亡等事件密切相关。该激动胶束为绝大多数失去溶栓治疗机会的缺血性脑卒中患者提供了新的替代性治疗策略。
Title:Edaravone-Encapsulated Agonistic Micelles Rescue Ischemic Brain Tissue by Tuning Blood-Brain Barrier Permeability.Doi:10.7150/thno.18219
Abstract: Thrombolysis has been a standard treatment for ischemic stroke. However, only 2-7% patients benefit from it because the thrombolytic agent has to be injected within 4.5 h after the onset of symptoms to avoid the increasing risk of intracerebral hemorrhage. As the only clinically approved neuroprotective drug, edaravone (EDV) rescues ischemic brain tissues by eradicating over-produced reactive oxygen species (ROS) without the limitation of therapeutic time-window. However, EDV's short circulation half-life and inadequate cerebral uptake attenuate its therapeutic efficacy. Here we developed an EDV-encapsulated agonistic micelle (EDV-AM) to specifically deliver EDV into brain ischemia by actively tuning blood-brain barrier (BBB) permeability. The EDV-AM actively up-regulated endothelial monolayer permeability in vitro. HPLC studies showed that EDV-AM delivered more EDV into brain ischemia than free EDV after intravenous injection. Magnetic resonance imaging also demonstrated that EDV-AM more rapidly salvaged ischemic tissue than free EDV. Diffusion tensor imaging indicated the highest efficiency of EDV-AM in accelerating axonal remodeling in the ipsilesional white matter and improving functional behaviors of ischemic stroke models. The agonistic micelle holds promise to improve the therapeutic efficiency of ischemic stroke patients who miss the thrombolytic treatment.
Webpage: http://www.thno.org/v07p0884